Lesson 2: Practical Management of Infant Feedings
2.4 Human Milk Fortifiers
As seen in the previous part of this lesson, while HM is considered the best feeding choice for preterm infants, fortification is needed for adequate intake of protein, energy, vitamins, minerals and micronutrients (Ziegler 2014). Including also carbohydrates and/or lipids, fortifiers can also increase the caloric density of the milk while keeping the feeding volume low.
Human milk fortifiers (HMFs) normally contain proteins, fat and carbohydrates. Protein is an important nutrient in the composition of HMFs. Providing enough proteins to the preterm infant is crucial. Because growth and neurodevelopment are associated with protein intake, the supply of protein must be constant and available at all times. However, in other to avoid adverse metabolic effects, over supply should also be avoided.
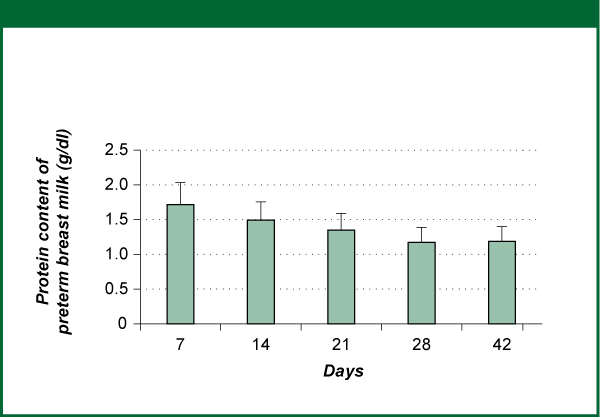
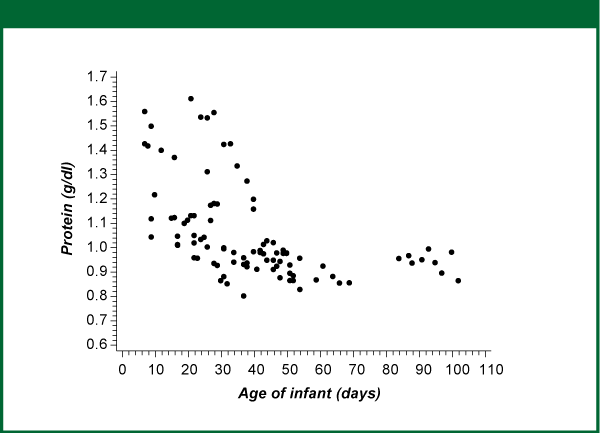
Fortification of HM is not an easy task, mainly because human milk protein content can vary considerably. Protein content decreases dramatically with lactation time (Figure 1). In addition, protein concentrations in HM can also be strikingly different from mother to mother (Figure 2) (Ziegler 2014).
Figure 1. Protein concentration of milk expressed by mothers of premature infants
Means and SD. Data represent true protein
Source Ziegler 2014, reprinted with permission of S. Karger AG, Switzerland
Figure 2. Protein concentration of milk expressed by mothers
of premature infants.
Each symbol represents protein concentration of a pool
of milk intended for consumption over 24 h.
Protein obtained as total nitrogen × 0.83 × 6.25
Source: Ziegler 2014; reprinted with permission of S. Karger AG, Switzerland
Currently, available HM fortifiers are able to provide the preterm infant with adequate nutrient content with the exception of proteins (Table 6). Fortifiers are available as powder or liquid. Normally, they are commercialized in premeasured sachets or vials, which will be added to a predetermined volume of HM (normally 25 ml). Their composition can vary considerably. Fortifiers can be produced either with cow's milk protein (either partially hydrolyzed or intact) or human milk's protein.
General protein provision in fortifiers:
- Powder fortifiers: 1.0-1.1 g protein/dl milk
- Cow`s milk based liquid protein fortifiers: 1.0-1.8 g protein/dl milk
- Human milk protein liquid fortifier: 0.6g protein /dl (when used at 80 kcal/dl); 1.5g protein /dl (when 1 part of fortifier added to 1 part milk, resulting in caloric density of 100 kcal/dl).
Table 6 Nutrient requirements of infants weighing <1000g (expressed per kg/day and per 100 kcal) versus typical composition (per kcal) of unfortified human milk at 4 weeks of lactation, and typical milk fortified with a powder fortifier that adds 1.0g of protein per 100ml of milk.
As seen in Table 6, fortifiers fall short in providing preterm infants with enough protein to supply minimal requirements. The reason that fortifiers tend to undershoot the actual requirements for preterm infants has to do with a fear of providing too much protein when added to expressed human milk (Ziegler 2014). This fear arose following publication of a 1974 study (Goldman et al. 1974) that found significantly lower IQs in children born <1300g who had received an infant formula with very high content (6.0-7.2g per kg/day) of a low-quality protein (casein-predominant cow's milk protein) while in the neonatal care unit.
In addition, there has also been a tendency to overestimate the average protein content of preterm human milk and to disregard the drop in protein that occurs in the later weeks of lactation (Miller et al. 2012). This has further contributed to the frequently inadequate protein intakes provided by fortified milk. The actual level at which a high protein supply may become harmful has never been defined. At the same time, there is now ample evidence that the smallest preterm infants fed with standard available preparations (fortifiers in human milk or preterm formulas) are at very high risk for poor growth due to insufficient dietary protein.
In a randomized controlled trial (RCT) with 92 infants born at <31 weeks, (Miller et al. 2012) compared 43 human milk fed infants receiving a fortifier providing 1.4 g/100ml to 49 infants receiving a fortifier providing 1.0 g/100ml. The infants in the higher-protein group had significantly less growth faltering by discharge or expected date of delivery (whichever came first). Similar encouraging results were seen by Moya and colleagues, who maximized protein intakes and minimized human milk dilution using an ultraconcentrated liquid fortifier (Moya et al. 2012).
For that reason, some manufactures are now producing higher-protein or ultraconcentrated fortifiers to provide more protein. Protein supplements in powder or liquid form can also be used, possibly in combination with milk analysis, to "customize” the protein content of fortified milk (Ziegler 2014). This approach however is not commonly practiced, since bedside milk analyzers are still not approved for clinical use in many countries including the USA.
The AAP, the WHO and the ESPGHAN recommend the use of HMFs in premature infants born weighing less than 1.5 kg (AAP 2012, WHO 2011, Agostoni et al. 2010). However, practical experience has shown that it may be desirable to extend the recommendations on human milk fortification also for heavier preterm infants. Many NICUs around the world adopt the use of HMF for infants weighing less than 2000 g and those infants being fed non-fortified human milk who show growth faltering.
The optimal point at which human milk fortifiers should be introduced has not been definitively established. Generally HMFs have been added when infants are tolerating feeding volumes of 50-100 ml/kg/day, but a recent study (Tillman et al. 2012) showed no adverse effects and a lower alkaline phosphate level in infants who received HMF with the onset of enteral feeds.