Lesson 6: Home Setting: Post-discharge Feeding and Monitoring
6.2 Current guidelines for feeding the preterm infant after discharge
Despite the difficulty in making generalizations about the post-discharge care of preterm infants, most experts and expert organizations agree on two points. First, human milk, if available, is the feeding of choice for all infants, including those born preterm. Second, preterm infants require a close follow-up and monitoring of their growth and development (Lapillonne 2014).
Although human milk is the feeding of choice, preterm infants are at particularly high risk of breastfeeding failure. This is due to the difficulties that many preterm infants experience with coordinating their suck and swallow in order to extract milk effectively from the breast, the lesser strength and stamina of preterm infants relative to term infants, and the challenge for mothers of preterm infants to establish and maintain an adequate milk supply.
The ESPGHAN Committee on Nutrition in 2006 released guidelines about feeding after discharge (Aggett et al. 2006) stating that preterm infants ....
" discharged home with normal weight for post-conceptional age are not at increased risk of long-term growth failure and could be fed similarly to term infants of similar gestational age. By contrast, those with subnormal weight for post-conceptional age are at increased risk of long-term growth failure and require particular attention and follow-up”. (Lapillonne 2014)
ESPGHAN also include in their guidelines that breastfeeding and fortified human milk should be promoted. Additionally, the use of preterm formula or a special post-discharge formula (with higher protein, minerals, trace elements and LC-PUFAs concentrations than term infant formula) is encouraged when the infant is either exclusively formula-fed or breastfed with formula supplementation. These special infant formulas should be used until the preterm infant reaches 40 weeks' post-conceptional age or in particular cases up to 52 weeks' post-conceptional age (Lapillonne 2014).
The AAP in their most recent edition of the Pediatric Nutrition Handbook also supports the use of special preterm infant formulas after discharge instead that of normal term formulas (Kleinman & AAP 2009).
Nutrient- enriched Human milk
 Preterm infants with suboptimal growth by the time of discharge should receive fortified human milk to get adequate nutrient supply for normal development (Aggett et al. 2006). However, very little research has been carried out to assess the beneficial effects of such practice.
Preterm infants with suboptimal growth by the time of discharge should receive fortified human milk to get adequate nutrient supply for normal development (Aggett et al. 2006). However, very little research has been carried out to assess the beneficial effects of such practice.
Two studies address the fortification of human milk for preterm infants after hospital discharge. These are summarized in a Cochrane review (Young et al. 2013). The first study involved 39 predominantly human milk fed infants with a birth weight between 750-1800g. The control group (unfortified human milk) compared to the intervention group (1/2 human milk feeds nutrient-enriched) showed a significantly smaller weight, length and bone mineral content both at 12 weeks, with effects persisting at 1 year. The smaller infants in the intervention group (birth weight <1250g) also showed sustained significantly greater head circumferences than the infants in the control group (Aimone et al. 2009). In contrast, a larger study of over 300 predominantly human milk-fed preterm infants by Zachariassen and collaborators (Zachariassen et al. 2011) did not demonstrate a significant growth benefit at 12 months' corrected age following addition of a milk fortifier to breast milk from discharge until 4 months' corrected age.
The Cochrane review observed no clear significant effect of fortifying human milk for preterm infants. No differences in weight or head circumference during the first year of life but a positive effect in length was seen at 12 months (Young et al. 2013).
Nutrient-enriched Formula
A Cochrane review published in 2012 (Young et al. 2012) reviewed the benefits of feeding preterm infants after discharge with nutrient-enriched formulas compared to standard term formulas. Nutrient-enriched formulas included were preterm specific formulas with energy content >75 kcal/100ml and protein content greater than 2.0 g/100 ml, and post-discharge formulas with energy content between 72 to 75 kcal/100 ml and protein content greater than 1.7 g/100ml. The controls' standard formulas had energy content between 66-68 kcal/ml and 1.4-1.5 g/100 ml of proteins.
They observed and concluded that the use of post-discharge formulas did not show significant beneficial effects compared to standard term formulas. However, it is noteworthy that preterm infants at highest nutritional risk were excluded or underrepresented in these trials (i.e. a very small cohort of SGA infants). When analyzing infants with growth restriction at birth, the use of post-discharge formulas showed a significant effect in length and head circumference.
The use of preterm infant formula after discharge, however, showed higher rates of growth when compared to the use of standard term formulas. Preterm formula-fed infants were approximately 500g heavier and 5 to 10 mm taller than term formula-fed infants at 12 to 18 months corrected age. Additionally, head circumference in the preterm formula-fed infants was around 5 cm larger than term formula fed infants from 6 to up 18 months corrected age.
There is also evidence that nutrient- enriched formulas do not generate central adiposity in preterm infants, despite increasing lean mass accretion and mineralization (Lapillonne 2014).
Table 15 shows the nutritional needs by weeks of gestation. Preterm infants after discharge should at least receive the respectively intake for their gestational age.
Table 15: Nutritional needs by weeks of gestation
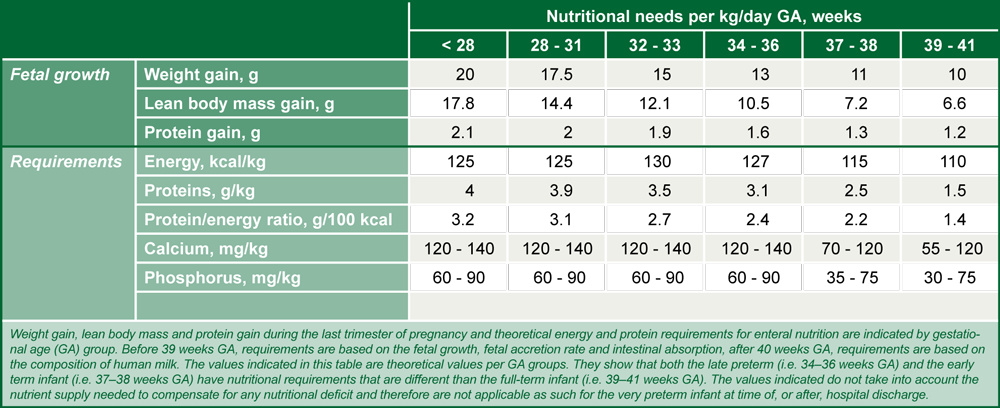
Source: Lapillonne 2014; reprinted with permission of S. Karger AG, Switzerland
Recommendations for continuing supplementation of specific nutrients following discharge
Provision of adequate protein and energy is central to the nutritional management of preterm infants and deficits will result in poor growth, which, in turn, may be associated with poorer neurodevelopmental outcomes. (Please see Unit 1 of this module for more information on growth and neurodevelopment.) Some other nutrient deficits, however, may be less readily apparent as they do not necessarily result in poor linear growth. At the same time, requirements for some nutrients are higher for preterm than for term infants. Recommendations exist for continuation of higher intakes of some nutrients following hospital discharge, as compared to usual supplies to healthy term infants.
Nutrients for bone health
Calcium, phosphorus and Vitamin D are important for bone mineralization. Osteopenia of prematurity can result when supplies are low, particularly during phases of rapid "catch-up” growth. Poor bone mineral content, which also occurs during growth spurts in adolescence, appears to be a self-resolving condition. Whether there are long-term consequences for bone health is not certain. Calcium and phosphorus requirements for preterm infants who are undergoing "catch-up” growth will likely be higher than for term infants. These higher requirements will probably be covered if the infant is consuming fortified human milk or special nutrient-enriched formula. A vitamin D intake of at least 400IU/day is generally recommended for both preterm and term infants (Wagner et al. 2008, Koletzko et al. 2014b). Evidence does not exist for higher dosing of vitamin D after discharge in preterm infants relative to term infants (Lapillonne 2014).
Iron
Iron-deficiency anemia is frequent in preterm infants, and iron supplementation begun in-hospital (refer to Unit 2 Lesson 7 - Microminerals) should be continued after discharge with a target intake in the range of 2-3 mg/kg/day (Baker et al. 2010; Koletzko et al. 2014b). Target intakes may be achieved through use of supplements or iron-enriched formulas or - after 6 months of age - through introduction of iron-rich complementary foods. Intermittent screening for iron deficiency is recommended.
LC-PUFAs
Preterm infants should receive supplementation with LC-PUFAs, as discussed in Unit 2 Lesson 5 of this module. The intakes recommended for preterm infants should be continued until the infant reaches 40 weeks post-menstrual age. Thereafter, supplementation is as for term infants (Lapillonne 2014).
Protein
Protein needs are closely related to growth rates. Since desirable weight gain of preterm infants at the time of discharge tends to be higher than that of infants born at term, protein needs are greater and are not well covered by human milk alone, nor by modern infant formula for term infants that have protein contents around 1.8-2 g/100 kcal. Therefore, for preterm infants that at the time of discharge are partially breastfed or formula-fed, it appears desirable to use preterm formula where feasible that are enriched with certain nutrients, relative to contents typically found in infant formula for term infants, such as calcium, phosphorus, vitamin D, iron, LC-PUFA and protein.