Lesson 9: Vitamins
9.2.2 Fat-soluble Vitamins - Vitamin D
 The history of vitamin D goes back to the 17th century when Whistler (in 1645) and Glisson (in 1650) described rickets as a bone disease of young children. However it was only in the beginning of the 20th century that vitamin D was finally identified and characterized (reviewed by Rajakumar 2003).
The history of vitamin D goes back to the 17th century when Whistler (in 1645) and Glisson (in 1650) described rickets as a bone disease of young children. However it was only in the beginning of the 20th century that vitamin D was finally identified and characterized (reviewed by Rajakumar 2003).
Vitamin D is normally found in fatty fish livers, and recently a number of foods have been vitamin D fortified (milk, orange juice, cereals, etc). Most vertebrates synthetize vitamin D in their skin under the influence of UVB light (Holick & Clark 1978). Therefore, a major source of vitamin D is through dermal synthesis. An efficient sun exposure of 2 hours per week of face and hands is probably sufficient for maintaining normal levels. The production of vitamin D3 in the skin does not require an enzyme (Figure 12). Skin exposure to UVB light produces D3 (cholecalciferol) from 7-dehydrocholesterol in a two-step process. Although this process is highly efficient, UVB intensity and skin pigmentation modulates D3 synthesis (Bikle 2014).
In the liver, the hepatic enzyme 25-hydroxylase is responsible for the formation of 25-hydroxyvitamin D (25(OH)D). The 25-hydroxyvitamin D then travels through the blood linked to the vitamin D-binding protein to the kidney. There, the enzyme 1α-hydroxylase finally can produce 1,25-dyhydroxyvitamin D3, which is the active form of vitamin D (figure12).
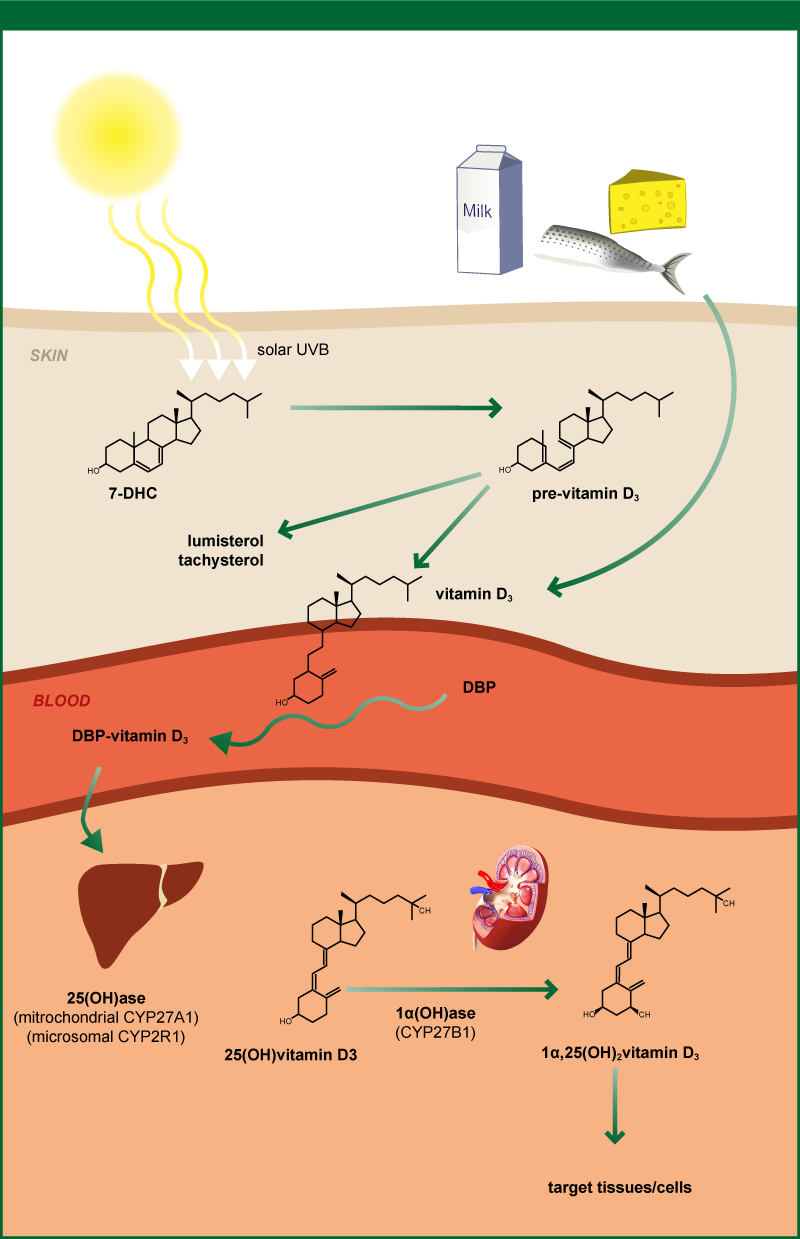
Figure 12. Vitamin D metabolism
Source: adapted from Mathieu et al. 2005
Vitamin D stores at birth
25(OH)D is the major circulating vitamin D metabolite and it is in this form that vitamin D is transferred to the fetus through the placenta. Being a fat soluble vitamin, vitamin D stores at birth would be expected to be lower in preterm infants than term infants. Therefore, preterm infants are at risk of vitamin D deficiency (Dawodu & Nath 2011, Natarajan et al. 2014). Monangi and colleagues described a 64% presence of Vitamin D deficiency (serum 25(OH)D <50 nmol/L) in preterm infants born before 32 weeks of age (Monangi et al. 2014). In a prospective study including 471 infants born in Boston, preterm infants (<32 weeks) had an increased risk of low 25(OH)D levels (<20 ng/ml) as compared to more mature infants (Burris et al. 2014). Vitamin D status at birth is totally dependent on maternal serum concentration (Dawodu & Nath 2011, Monangi et al. 2014, Kovacs 2008).
Vitamin D dermal synthesis
Since preterm infants are usually not exposed to UV light in the NICU, and they are unlikely to receive such exposure even after NICU discharge, UV- mediated vitamin D production is considered null in these infants (Mimouni et al. 2014).
Vitamin D metabolism in preterm infants
Preterm infants seem to have similar intestinal vitamin D absorption and metabolism as term infants (Mimouni et al. 2014). The liver 25-hydroxylase and the 1α-hydroxylase in kidney enzymes also appear to be effective in preterm infants. In addition, in a study by Koo and collaborators, the active form of vitamin D (1,25-dyhydroxyvitamin D3) when administrated to VLBW preterm infants triggered an appropriate calcemic response (Koo et al. 1986).
Based on the current evidence, vitamin D requirements for preterm infants should range between 400 to 1000 IU/day. Vitamin D status at birth should serve as a guideline for supplementation. In preterm infants with no vitamin D deficiency, 400 IU/day should be enough to maintain an adequate concentration of >50 nmol/l of 25(OH)D, prevent rickets and avoid the risk of intoxication. However, newborn preterm infants whom are vitamin D deficient should receive 1000 IU/day to normalize neonatal stores. It is not yet known though, if these supplementation values are enough to provide preterm infants with the vitamin D extraskeletal benefits. More investigation is therefore warranted (Mimouni et al. 2014).